Advancing Healthcare through Digital Twins and Simulation Modeling in the Middle East
Healthcare systems across the Middle East are experiencing a profound structural transformation. Historically, national healthcare progress was primarily measured by expanding hospital capacity, establishing specialty centers, and investing heavily in cutting-edge clinical infrastructure. These efforts have laid the foundation for world-class healthcare systems throughout the region. However, healthcare leaders today acknowledge that the forthcoming wave of transformation will not be driven by physical infrastructure alone. Instead, the intelligence embedded within healthcare systems—the data-driven insights, predictive capabilities, and interconnected technologies—will be the catalysts of change.
As countries across the Middle East transition into this new era, healthcare systems are increasingly capable of anticipating patient demand, simulating clinical outcomes, optimizing the allocation of scarce resources, and delivering personalized care at scale. Central to this evolution is the rapid adoption of digital twins and simulation modeling technologies. What were once conceptual tools have now become integral components of operational healthcare frameworks in Saudi Arabia, the UAE, Qatar, and several emerging healthcare markets in the region. These technologies empower healthcare providers to create virtual replicas of physical systems and processes, enabling dynamic scenario planning and real-time decision-making that enhance overall system efficiency and patient outcomes. This digital transformation signals a shift towards more intelligent, responsive, and patient-centric healthcare systems that will define the region’s future.
Critical Business Challenges Driving the Adoption of Digital Transformation in Middle Eastern Healthcare
The accelerating digital transformation across the Middle East is encountering critical business challenges that demand more than conventional digital records management or basic automation solutions. Healthcare systems in the region face complex structural issues that cannot be resolved through incremental improvements alone. Instead, these challenges call for advanced predictive management capabilities, enabling hospitals and healthcare providers to simulate potential decisions and their impacts before implementation. Digital twins are addressing this gap by offering powerful tools that allow healthcare organizations to test various scenarios, forecast clinical and operational outcomes, and optimize workflows across both clinical and non-clinical settings. By leveraging these technologies, healthcare systems can enhance decision-making precision, improve resource utilization, and ultimately deliver higher-quality, more efficient care in an increasingly complex environment.

Leveraging Digital Twin Technology to Address Regional Challenges
Digital twins bring capabilities that align directly with national healthcare strategies across the region:
-
Real-time monitoring of patient, hospital, and system activity
-
Prediction of clinical risks and care-pathway bottlenecks
-
Simulation of capacity needs and resource allocation
-
Integration of clinical, operational, and energy-management systems
-
Scenario-testing for national health planning
The region’s investment in AI, 5G, national interoperability platforms, and cloud infrastructure has created ideal conditions for digital twins to move beyond pilots and into routine operations.
We are already seeing deployments that support ICU-capacity forecasting, surgical scheduling optimization, patient-flow modelling, AI-assisted diagnostics, and hospital energy optimization — especially across Saudi Arabia and the UAE.
Below is a consolidated view of how Middle Eastern countries are deploying digital twins across patient, hospital, network, and national levels.
|
Category |
Country |
Example |
Description / Analyst Note |
|
Patient-Level Digital Twins |
Saudi Arabia |
Sehhaty Digital Health Twin |
Launched October 2024; world’s largest health twin platform (>30M users). Creates virtual versions of individuals using clinical + wearable + lifestyle data to predict NCD risks and simulate health trajectories. |
|
UAE |
Dr. Mansoor’s Digital Twin Doctor |
A digital twin of Dr. Mansoor Al-Zaabi. Uses voice cloning + AI for preventive wellness guidance in 30+ languages; 24/7 health awareness support. |
|
|
Network-Level Digital Twins |
Saudi Arabia |
Seha Virtual Hospital Network |
Connects 170+ hospitals. Uses AI-driven diagnostics, remote monitoring, and resource-optimization algorithms. Strongest network-level twin in Middle East. |
|
Hospital & Facility-Level Twins |
Kuwait |
Jaber Hospital – AI Surgical & ICU Integration |
Uses advanced AI imaging, 3D organ visualization, and intra-operative decision tools—considered a stepping stone toward full hospital-level twins. |
|
Qatar |
Hamad & Sidra Medical Centers – Operational Twin Pilots |
Running pilots for ICU bed-capacity forecasting, surgical scheduling optimization, and hospital-operation simulations. |
|
|
National/System-Level Digital Twins |
Saudi Arabia (NEOM) |
City-Scale Digital Twin Ecosystem |
NEOM is building a real-time, city-wide digital twin integrating health, environment, mobility, and infrastructure—most advanced transformation-stage model in ME. Healthcare will run predictive, autonomous workflows. |
These examples highlight momentum across all layers of the digital-twin stack: patient → hospital → network → city/nation.
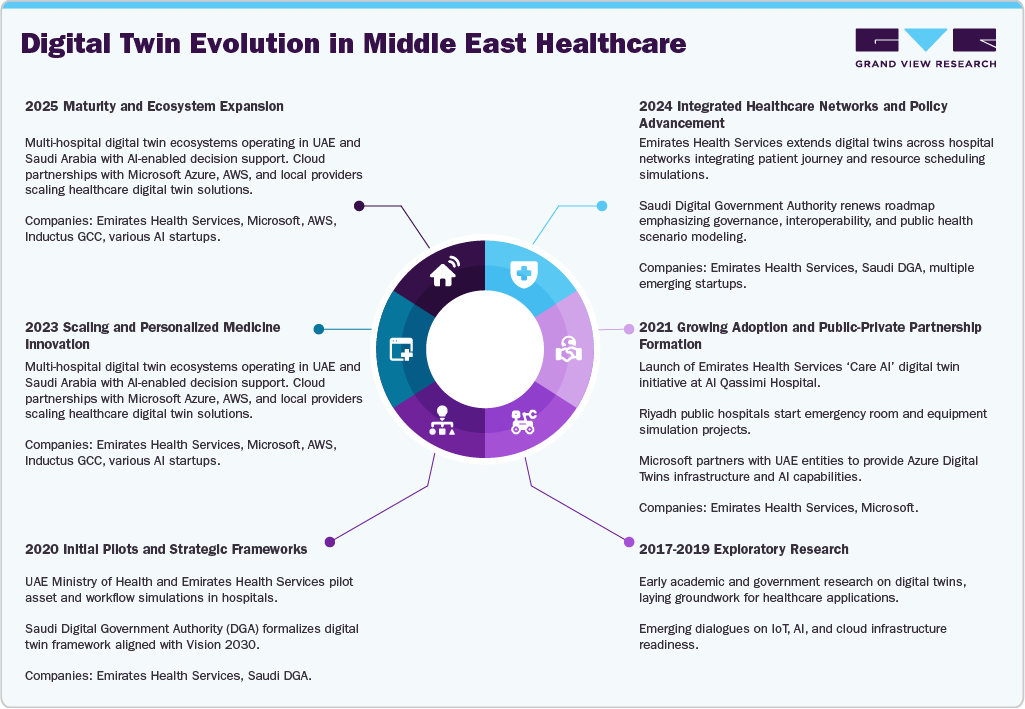
Digital Twin Lifecycle: Country Readiness in the Middle East
Understanding each country’s position in the digital twin lifecycle is crucial for aligning investment decisions with local readiness.
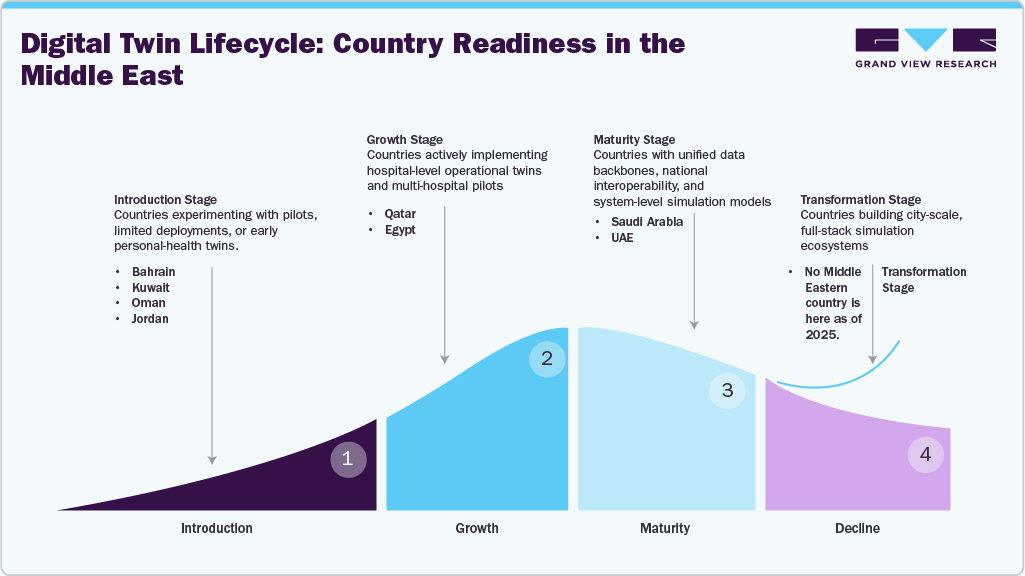
The table below summarizes each country’s placement in the lifecycle, reflecting differences in digital-health maturity, interoperability, pilot activity, and readiness for large-scale simulation adoption.
|
Lifecycle Stage |
Country |
Analyst Notes |
|
Introduction Stage |
Bahrain |
Early-stage pilots and exploratory collaborations (e.g., discussions to connect with Saudi’s Seha Virtual Hospital). Limited hospital-level or national twin deployments. |
|
Kuwait |
Jaber Hospital is adopting AI-driven visualization in surgeries, but full digital twin frameworks are not deployed; activity remains foundational and exploratory. |
|
|
Oman |
Slow digital modernization, limited EMR standardization, and no formalized digital twin initiatives beyond basic digital health upgrades. |
|
|
Jordan |
Strong clinical infrastructure but early-stage digital transformation. Pilots are fragmented and largely vendor-led rather than system-led. |
|
|
Growth Stage |
Qatar |
Running multi-hospital pilots (Hamad & Sidra Medical Centers) for ICU simulation and surgical optimization. National E-Health Program strengthens data integration foundations. |
|
Egypt |
Rapid health digitization, but projects remain pilot-level. Large system complexity and fragmented EMR environments place Egypt in scaling–but not mature–adoption. |
|
|
Maturity Stage |
Saudi Arabia |
Most comprehensive national digital twin ecosystem in the region: Sehhaty personal twin (30M+ users), Seha Virtual Hospital network (170+ hospitals), and NPHIES interoperability backbone. Near-system-level simulation readiness. |
|
UAE |
Operational digital twin at Al Qassimi Hospital (EHS), strong AI governance, and advanced health-tech pilots across emirates. Integrated, scalable architecture places UAE in early maturity. |
|
|
Transformation Stage (Future State) |
No Middle Eastern country as of 2025 |
City-scale, fully autonomous simulation ecosystems (like NEOM’s future model) are still in development. No country has population-wide real-time health twins or fully unified clinical–operational–insurance twin environments. |
Country-Level Progress & Market Signals
UAE: EHS Operational & Energy Twin
EHS, with Microsoft and Schneider Electric, deployed a hospital digital twin at Al Qassimi Hospital linking building systems, HVAC, and energy data. Early results show:
-
~30% reduction in energy consumption
-
~20% fewer maintenance disruptions
This is one of the first Middle Eastern examples of combining clinical and non-clinical systems into a single simulation environment directly supporting the UAE’s 2031 strategy.
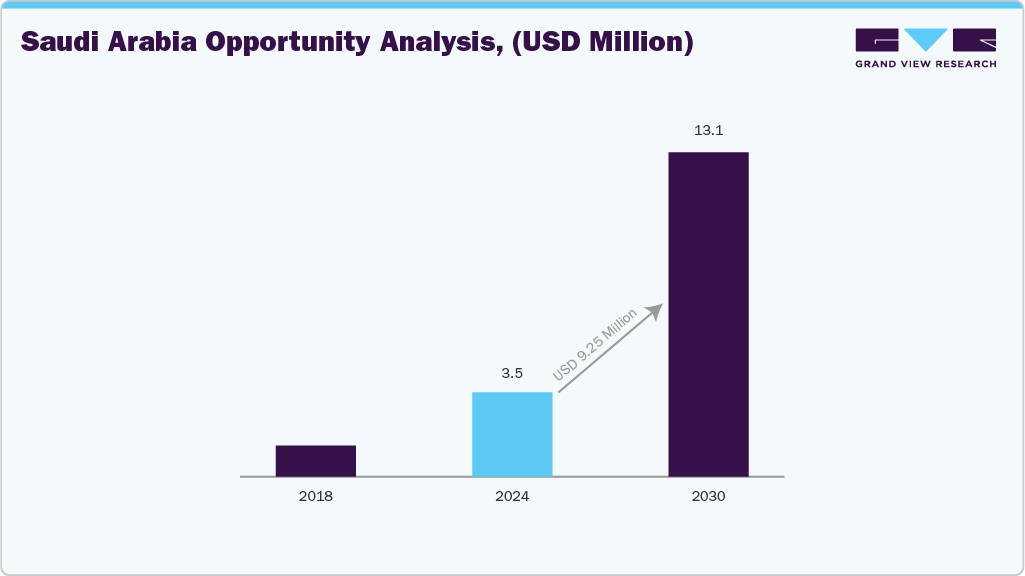
Saudi Arabia – Market Sizing Outlook for Digital Twins (2023–2030)
Saudi Arabia is shaping the digital twin landscape through Vision 2030 investments and a fully integrated digital-health infrastructure.
With more than 224 hospitals connected and 30+ million residents on Sehhaty, the Kingdom is:
-
Simulating patient trajectories
-
Optimizing multi-site workflows
-
Enhancing tele-diagnostics
-
Deploying AI-assisted remote care
Saudi Arabia is expected to be the largest and fastest-growing digital twin market in the Middle East through 2030.
Acceleration Toward Predictive Healthcare Ecosystems by 2030
By 2030, digital twins will become a foundational layer across Middle Eastern healthcare systems. The region is moving toward:
-
Patient-specific clinical and surgical twins for precision interventions
-
Hospital-wide operational twins integrating workflow, energy, and capacity planning
-
Population-health twins to forecast disease trends and manage emergencies
-
AI surveillance models to identify risks before clinical deterioration
KOL Insight: As one Saudi consultant surgeon noted, “simulation is no longer future tech — it is becoming everyday clinical decision support.” This aligns directly with the region’s shift toward smart, prevention-driven ecosystems.
Analyst View: What’s Ahead After 2025
Digital twins have moved from pilot experiments to national programs. Over the next five years, initiatives such as the UAE’s EHS Care-AI, Saudi Arabia’s DGA-led digital-health standards, and NEOM’s cross-sector twin ecosystem will push adoption from project-level to platform-level.
KOL Perspective: A UAE digital-health leader emphasized that “the challenge now isn’t AI — it’s harmonizing the data across systems.” This reinforces why interoperability, and governance will determine how quickly large-scale simulation becomes a system-wide capability.
Energy and workflow gains are also driving adoption; a Qatar hospital operations director highlighted that “when hospitals see a 20–30% cut in waste and disruptions, digital twins shift from innovation to ROI.”
As a result, digital twins will increasingly anchor clinical outcomes, operational efficiency, sustainability, and national planning into a unified predictive layer.
Key Takeaways for Middle Eastern Healthcare Leaders
-
Digital twins are a strategic asset, enabling precision care, operational optimization, and long-term system resilience.
-
Value is multi-layered—from patient treatment to hospital operations, capital planning, emergency preparedness, and national health management.
-
Scaling requires governance: interoperable data platforms, consistent standards, and clear regulatory direction.
-
Regional talent development is essential, including simulation engineers, digital twin architects, and clinical-analytics teams.
-
Payment models must evolve to reward predictive care, early intervention, and efficient resource utilization.
-
Cross-sector partnerships—public health authorities, hospitals, and technology vendors—will be the main accelerators of successful adoption.