- Home
- »
- Healthcare IT
- »
-
Healthcare Fraud Analytics Market Size Report, 2030GVR Report cover
![Healthcare Fraud Analytics Market Size, Share & Trends Report]()
Healthcare Fraud Analytics Market Size, Share & Trends Analysis Report By Solution Type (Descriptive, Predictive, Prescriptive), By Delivery Model, By Application, By End User, By Region, And Segment Forecasts, 2022 - 2030
- Report ID: GVR-4-68039-924-0
- Number of Pages: 150
- Format: Electronic (PDF)
- Historical Range: 2017 - 2020
- Industry: Healthcare
Report Overview
The global healthcare fraud analytics market size was valued at USD 1.63 billion in 2021 and is estimated to expand at a compound annual growth rate (CAGR) of 24.3% from 2022 to 2030. The increasing penetration of health insurance, coupled with the rising number of fraud cases in the healthcare industry, are factors driving the market growth. Furthermore, the growing focus on curbing healthcare costs, as well as the technological advancements to launch advanced analytical techniques, are also expected to fuel the market growth.
According to IBM Security’s X-Force Threat Intelligence Index, during the COVID-19 pandemic, the number of breached records and the severity of these breaches grew exponentially, despite an overall decline in the number of breach incidents across private and public sectors. This resulted in the adoption of healthcare fraud analytics software and services during the pandemic as well, hence supporting the market growth in 2020 and 2021.
As per the National Healthcare Anti-Fraud Association, every year payers spend nearly USD 68 billion due to fraud in the U.S. The risk of a nonexistent or unnecessary medical service owing to misrepresentation by providers or patients becomes an expensive investment.
Instead of investing in seeking out the bad areas, clinicians and medical consultants can focus on improving access to resources for chronic and urgent care, which can improve the quality of care by using data science, machine learning, and artificial intelligence-based solutions. Thus, the adoption of technologically advanced solutions drives the market growth.
According to an article published by Elsevier Inc., more than USD 700 billion are lost due to fraud, waste, or abuse in the healthcare system of the U.S. One of the most vulnerable targets for fraud in the past few years has been Medicaid. This is due to limited cross-program communication, a distributed management model, and a difficult-to-track patient population of low-income adults & their children. The use of effective fraud analytics solutions can help in curbing these high costs, thus boosting the market growth during the projection period.
Illegal medical billings with falsified claims, filing of multiple claims by different providers for the same patient, patient identity thefts & use for gaining reimbursement, and collusion between unprincipled providers & their patients, are some of the common healthcare fraud examples. According to a GAO report published in 2016, around 68% of all healthcare frauds are due to false billings and the providers are complicit in 62% of these cases, while patients are complicit in 14% of them. Such factors are expected to fuel the demand for advanced healthcare fraud analytics solutions.
Solution Type Insights
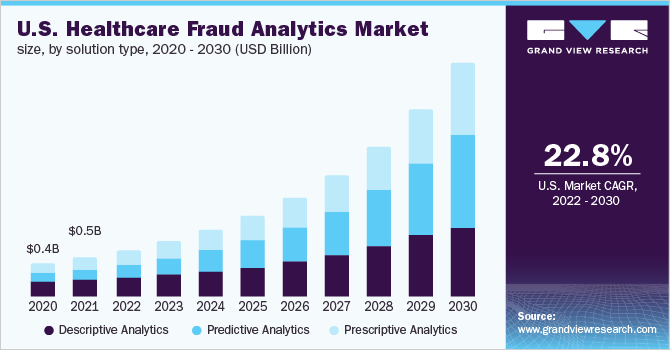
The descriptive analytics segment held the largest market share of around 40.0% in 2021, owing to its high adoption due to ease of use. It utilizes current as well as historical data for the identification of trends and relationships. This helps in the identification of possible frauds in a better way. It also acts as a base for an effective application of prescriptive and predictive analytics. This further supports the segment’s growth.
The predictive analytics segment is anticipated to witness the fastest growth during the projected period. The most effective way for preventing fraud is by identifying them before the claims are paid. Owing to this, healthcare payers have started adopting predictive analytics solutions. These solutions identify the patterns that are potentially fraudulent, and then develop some rules to flag certain claims.
The prescriptive analytics segment is also expected to witness significant growth, as they also help in evaluating the cost and benefit of a certain solution and help them organize to analyze if they are spending more on trying to catch the fraud, as compared to what they would be losing from the potential fraud.
Delivery Model Insights
The on-premise segment held the highest revenue share of more than 51% in 2021, owing to the ease of access of data being on the site, i.e., hospitals, etc. which has resulted in better management of records as well as monitoring of the data, among other things. Current systems in small organizations are practical, but when scaled up it can be difficult and cumbersome to manage data if the organization is dealing with a large dataset. This can mean large capital investment in the storage and security of data.
The cloud-based segment is estimated to witness the fastest growth of 26.2% during the forecast period, as it has been the emerging delivery mode because it provides a larger space virtually to store data for a multitude of patients. This is cost-effective and is commercially a more viable option for industries. Limitations of this segment include more security concerns regarding loss of data and less privacy.
Application Insights
The insurance claims review segment held the largest market share of over 35% in 2021, due to the rising adoption of health insurance by people, which also results in a growing number of fraudulent claims. The segment is further divided into post-payment review and prepayment review. The prepayment review segment is likely to grow at the fastest CAGR owing to its rising demand from healthcare providers.
The pharmacy billing issue segment is also expected to grow significantly, owing to the rising number of medical billing frauds occurring in the pharmacies. Similarly, the payment integrity segment is also likely to expand at a considerable growth rate. Payment integrity is a tool, which payers use for tightening the administrative side to lower the costs.
End-User Insights
By end-user, public & government agencies dominated with a share of over 41.0% in 2021 in the healthcare fraud analytics market. The key factors contributing to the large share include a higher volume of patients in government hospitals, and the high vulnerability of government agencies to fraudulent activities due to the lack of technologically advanced infrastructure, especially in the developing nations.
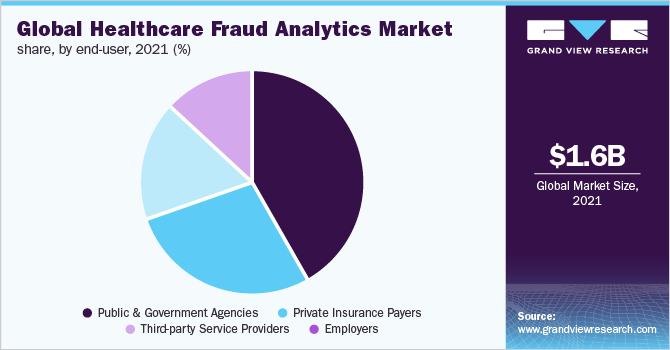
The employers' segment is anticipated to grow at the highest CAGR during the projected period, owing to the increasing demand for healthcare fraud analytics by employers for enabling better cost management. The private insurance payers segment is also estimated to witness significant growth, owing to the rising use of fraud analytics solutions for combating the growing monetary losses.
Regional Insights
North America dominated the global market with a share of around 38% in 2021. This is owing to the rising healthcare spending, increasing healthcare IT adoption, and the growing number of fraud cases. According to data published by the National Library of Medicine, fraudulent activities are more commonly seen in the North America region, followed by Europe and Asia Pacific region, in the year 2020. Asia Pacific region is likely to witness the fastest growth rate of around 26.7% during the projected period, owing to the increasing adoption of technologically advanced solutions.
According to National Health Care Anti-Fraud Association (NHCAA), the United States spends over USD 2.27 trillion on health care every year. Of that amount, NHCAA estimates that tens of billions of dollars are lost to health care fraud. Thus, owing to the availability of numerous advanced services and solutions related to healthcare fraud detection, and strategic steps taken by major players present in the country, it is expected to drive the growth of the studied market in the North America region during the projection period.
Key Companies & Market Share Insights
The market for healthcare fraud analytics is competitive. Key companies deploy strategic initiatives, such as product development and launches, sales & marketing strategies to increase product awareness, regional expansion, and partnerships to strengthen their market share. For instance, in December 2021, Wipro Limited acquired LeanSwift. This acquisition has expanded the capabilities of Wipro FullStride Cloud Services. Some of the key players in the global healthcare fraud analytics market include:
-
IBM
-
Optum, Inc.
-
Cotiviti, Inc
-
DXC Technology
-
SAS Institute, Inc.
-
EXL Service Holdings, Inc.
-
Wipro Limited
-
Conduent, Inc
-
HCL Technologies Limited
-
OSP Labs
Healthcare Fraud Analytics Market Report Scope
Report Attribute
Details
The market size value in 2022
USD 1.97 billion
The revenue forecast in 2030
USD 11.23 billion
Growth Rate
CAGR of 24.3% from 2022 to 2030
Base year for estimation
2021
Actual estimates/Historical data
2017 - 2020
Forecast period
2022 - 2030
Quantitative units
Revenue in USD million & CAGR from 2022 to 2030
Report coverage
Revenue forecast, company ranking, competitive landscape, growth factors, and trends
Segments covered
Solution type, delivery model, application, end-user, region
Regions covered
North America; Europe; Asia Pacific; Latin America; MEA
Country Scope
U.S.; Canada; U.K.; Germany; Italy; France; Spain; Japan; China; India; Australia; South Korea; Brazil; Mexico; Argentina; South Africa; Saudi Arabia; UAE
Key companies profiled
IBM; Optum, Inc.; Cotiviti, Inc.; DXC Technology; SAS Institute, Inc.; EXL Service Holdings, Inc.; Wipro Limited; Conduent, Inc.; HCL Technologies Limited; OSP Labs
Customization scope
Free report customization (equivalent up to 8 analysts’ working days) with purchase. Addition or alteration to country, regional & segment scope.
Pricing and purchase options
Avail customized purchase options to meet your exact research needs. Explore purchase options
Segments Covered in the Report
This report forecasts revenue growth at the global, regional & country levels and provides an analysis of the latest industry trends and opportunities in each of the sub-segments from 2017 to 2030. For this report, Grand View Research has segmented the global healthcare fraud analytics market report based on solution type, delivery model, application, end-user, and region:
-
Solution Type Outlook (Revenue, USD Million, 2017 - 2030)
-
Descriptive Analytics
-
Prescriptive Analytics
-
Predictive Analytics
-
-
Delivery Model Outlook (Revenue, USD Million, 2017 - 2030)
-
On-premises
-
Cloud-based
-
-
Application Outlook (Revenue, USD Million, 2017 - 2030)
-
Insurance Claim Review
-
Postpayment Review
-
Prepayment Review
-
-
Pharmacy billing Issue
-
Payment Integrity
-
Others
-
-
End User Outlook (Revenue, USD Million, 2017 - 2030)
-
Public & Government Agencies
-
Private Insurance Payers
-
Third-party Service Providers
-
Employers
-
-
Regional Outlook (Revenue, USD Million, 2017 - 2030)
-
North America
-
U.S.
-
Canada
-
-
Europe
-
Germany
-
U.K.
-
France
-
Italy
-
Spain
-
-
Asia Pacific
-
China
-
India
-
Japan
-
Australia
-
South Korea
-
-
Latin America
-
Brazil
-
Mexico
-
Argentina
-
-
MEA
-
South Africa
-
Saudi Arabia
-
UAE
-
-
Frequently Asked Questions About This Report
b. The global healthcare fraud analytics market size was estimated at USD 1.63 billion in 2021 and is expected to reach USD 1.97 billion in 2022.
b. The global healthcare fraud analytics market is expected to grow at a compound annual growth rate of 24.3% from 2022 to 2030 to reach USD 11.23 billion by 2030.
b. North America dominated the healthcare fraud analytics market with a share of 38% in 2021. This is attributable to rising healthcare spending, increasing healthcare IT adoption, and the growing number of fraud cases.
b. Some key players operating in the healthcare fraud analytics market include IBM, Optum, Inc., Cotiviti, Inc., DXC Technology, SAS Institute, Inc., Exlservice Holdings, Inc, Wipro Limited, Conduent, Inc, HCL Technologies Limited, and OSP Labs, among others.
b. Key factors that are driving the healthcare fraud analytics market growth include the increasing penetration of health insurance coupled with the rising number of fraud cases in the healthcare industry and technological advancements.
Share this report with your colleague or friend.
![gvr icn]()
NEED A CUSTOM REPORT?
We can customize every report - free of charge - including purchasing stand-alone sections or country-level reports, as well as offer affordable discounts for start-ups & universities. Contact us now
![Certified Icon]()
We are GDPR and CCPA compliant! Your transaction & personal information is safe and secure. For more details, please read our privacy policy.
We are committed towards customer satisfaction, and quality service.
"The quality of research they have done for us has been excellent."