- Home
- »
- Healthcare IT
- »
-
U.S. Business Process As A Service In Healthcare Payers MarketGVR Report cover
![U.S. Business Process As A Service In Healthcare Payers Market Size, Share & Trends Report]()
U.S. Business Process As A Service In Healthcare Payers Market Size, Share & Trends Analysis Report By Solution Coverage (Traditional BPaaS, Best-of-breed BPaaS), By Buyer Type, By Value Chain Processes, By Buyer Size, And Segment Forecasts, 2024 - 2030
- Report ID: GVR-4-68039-988-7
- Number of Report Pages: 92
- Format: PDF, Horizon Databook
- Historical Range: 2018 - 2022
- Forecast Period: 2024 - 2030
- Industry: Healthcare
Market Size & Trends
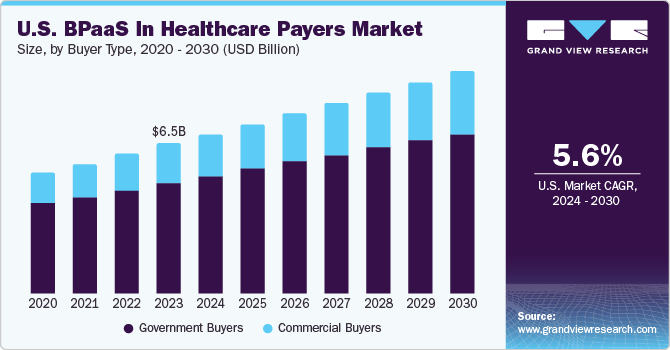
The U.S. business process as a service in healthcare payers market size was estimated at USD 6.5 billion in 2023 and is expected to grow at a compound annual growth rate (CAGR) of 5.62% from 2024 to 2030. The U.S. spends over USD 3.8 trillion on healthcare, which is roughly twice as much as any other major international economy, as a result of the complexity and inefficiency of its healthcare system. Business process as a service (BPaaS) engagements contribute significantly to payer business process outsourcing revenue, which is likely to drive the industry’s growth.
The U.S. healthcare industry is highly regulated. Healthcare payers are subjected to a complex web of regulations. The payer burden is also being exacerbated by a rapidly shifting regulatory environment and changing member demands. In addition, the Affordable Care Act and Centers for Medicare and Medicaid are establishing regulations and payment/reimbursement practices, causing more and more conversations. These pressures and the possibility of margins contracting make this an ideal time for payers to assess options for profitable growth and improved agility. Many healthcare payers are thus switching to the BPaaS model for planning administration, back-office functions, and others to focus on core activities.
The market is likely to be impacted by the COVID-19 pandemic, expanding healthcare consumerism, changing regulations, and shift to value-based care. Due to these challenges and declining margins, healthcare providers are being compelled to think about different game plans, such as BPaaS, to improve patient experience, which is eventually driving revenue growth due to rise in demand and acceptance of the BPaaS system.
The COVID-19 pandemic has greatly increased financial, regulatory, and technology challenges that healthcare payers currently confront. The pandemic has improved payers' cash flow in the short term, but it has also brought about major operational and market changes for which payers must get prepared. For instance, as per the Kaiser Family Foundation, enrollees under Medicaid grew by 32.6% from February 2020 to December 2022. The market is also anticipated to expand as a result of payers, including United Healthcare, Anthem, Centene, and Oscar Health, reviving their interest in this market due to changes in COVID-19's enrollment patterns.
Value Chain Processes Insights
Based on value chain processes, the market has been segmented into claims management, member engagement, care management, and others. The care management segment held a majority share of 31% in 2023 and is expected to retain its position during the forecast period. Care management enhances the efficiency of healthcare functioning while maximizing the benefits for healthcare institutes and patients. Care management is a proven way to increase the efficiency of healthcare operations while maximizing the advantages for both patients and healthcare institutions."
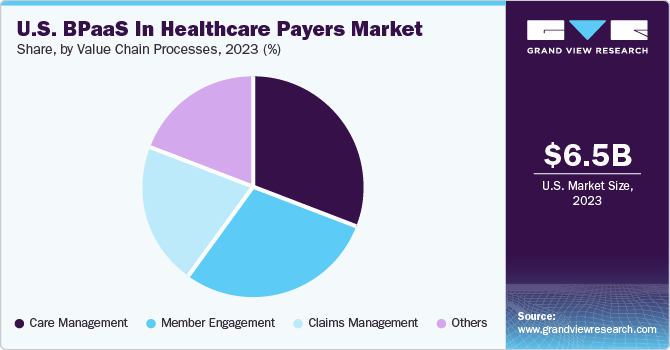
Others segment is anticipated to register maximum CAGR during the forecast period. This segment includes product development, network management, and risk & compliance. Insights gained from the data make it easier for payers to enhance the network and better serve patients and providers. Moreover, risk and compliance services in the insurance industry are increasingly aiming at adding value and utilizing technology to conduct activities more effectively and to drive efficiency.
Solution Coverage Insights
Based on solution coverage, the market has been segmented into traditional and best-of-breed. The traditional BPaaS segment has accounted for the largest market share of over 75% in 2023, owing to lower cost of service and higher customer satisfaction. Traditional business process outsourcing models are gradually shifting to the BPaaS model, an approach that focuses on total cost of ownership and pushes vendors to provide higher-value business outcomes. BPaaS alters focus and nature of engagement, resulting in more flexible and collaborative business partnerships focused on common goals.
The best-of-breed segment is anticipated to witness the fastest growth rate during the forecast period. Best-of-breed technology offers more data security for patient information and gives organizations an option to choose tools for specific services. Best-of-breed BPaaS models would be made possible by factors including expanding availability of BPS partner ecosystems for technological platforms and advancements in data security and compliance standards.
Buyer Type Insights
Based on buyer type, the government buyers segment held the majority of revenue share of over 73% in 2023. Government insurance companies have historically been the main buyers for BPaaS due to modular implementations of Medicaid Management Information Systems (MMIS). U.S. states have entrusted service providers with design, development, and implementation of MMIS platforms as well as use and maintenance of such platforms. As CMS advances its modularity agenda, more states are modernizing outdated monolithic systems and progressively moving to an as-a-service paradigm.
The outbreak of COVID-19 pandemic, already increased MA, and Managed Medicaid enrollment received an additional boost. According to a survey by MedicareAdvantagePlans.org, 45% of Medicare recipients will transfer from original Medicare plan to MA plan in 2021. In addition, the 21st Century Cures Act is anticipated to result in a significant increase in ESRD patients in MA plans. Commercial buyers segment is anticipated to witness considerable growth during the forecast period owing to an increasing number of people taking commercial insurance plans, which provide value-based services to beneficiaries.
Buyer Size Insights
Based on buyer size, the small buyers segment is estimated to dominate the market throughout the forecast period. Small buyers always have scope for innovations and help smaller insurers find niche opportunities for growth. A major benefit of midsized health plans is the provision of member-centric services. Any size payer can succeed if health insurance enrollment and claims processes are efficient.
The large buyers segment is expected to witness the fastest growth over the forecast period, as they can offer tactical administrative processes for achieving process efficiencies and enable major cost savings. Large health plans are closely monitoring developments, and increased adoption is expected in the long term as BPaaS solutions mature and more successful use cases emerge in the market.
Key Companies & Market Share Insights
Companies are stepping up their efforts to maintain their position in a competitively escalating market by introducing new products. For instance, Cognizant, which has a dominant position in the market for service providers to U.S. healthcare payers due to its industry knowledge, tools, cloud, and digital portfolio, invested USD 120 million in platform R&D in 2020 to support its BPaaS solutions. Additionally, Legato Health Technologies introduced a product business process as a service offering in 2021, enhancing its current portfolio of business process and technology services to better serve the requirements of health plans of all sizes.
Furthermore, companies that are primarily involved in this market and have strong BPaaS product offerings have increased their collaborations with providers in order to maintain their revenue share and support their U.S. operations. These partnerships enable partners to jointly develop cutting-edge programs, solutions, and initiatives for the benefit of patients and healthcare system. For instance, Genpact offers payers a strong BPaaS offering that grew out of its BPO legacy, an increasing emphasis on digital transformation skills, and an in-depth domain understanding in the healthcare sector.
Key U.S. Business Process As A Service In Healthcare Payers Companies:
- Accenture
- Cognizant
- HCL Technologies Limited
- IBM
- Infosys Limited
- NTT DATA Corporation
- Optum
- TATA Consultancy Services Limited
- UST
- Wipro
- EXL
- Softheon, Inc.
- Genpact
- Change Healthcare
- Firstsource
- Celegence
- Highmark Health
Recent Developments
-
In January 2021, Genpact acquired Enquero, a small California-based company that provides services for data engineering and data-led digital transformation, to strengthen its U.S. operations.
-
In November 2022, Halifax Health selected BPAS (a provider of retirement plans, fund administration, benefit plans, and collective investment trusts) for daily valuation recordkeeping of 10,000 participants in its defined contribution retirement plans.
U.S. Business Process As A Service In Healthcare Payers Market Report Scope
Report Attribute
Details
Revenue forecast in 2030
USD 9.6 billion
Growth rate
CAGR of 5.62% from 2024 to 2030
Base year for estimation
2023
Historical data
2018 - 2022
Forecast period
2024 - 2030
Report updated
November 2023
Quantitative units
Revenue in USD billion, and CAGR from 2024 to 2030
Report coverage
Revenue forecast, company ranking, competitive landscape, growth factors, and trends
Segments covered
Solution coverage, buyer size, buyer type, value chain processes
Country scope
U.S.
Key companies profiled
Accenture; Cognizant; HCL Technologies Limited; IBM; Infosys; NTT DATA Corporation; Optum; TATA Consultancy Services Limited; UST; Wipro; EXL; Softheon Inc.; Genpact; Change Healthcare; Firstsource; Celegence; Highmark Health
Customization scope
Free report customization (equivalent up to 8 analysts working days) with purchase. Addition or alteration to country, regional & segment scope.
Pricing and purchase options
Avail customized purchase options to meet your exact research needs. Explore purchase options
U.S. Business Process as a Service In Healthcare Payers Market Report Segmentation
This report forecasts revenue growth at the country level and provides an analysis of the latest industry trends in each of the sub-segments from 2018 to 2030. For this study, Grand View Research has segmented the U.S. business process as a service in healthcare payers market report based on solution coverage, buyer type, value chain processes, and buyer size:
-
Solution Coverage Outlook (Revenue, USD Billion, 2018 - 2030)
-
Traditional BPaaS
-
End-to-end Traditional BPaaS
-
Process-specific Traditional BPaaS
-
-
Best-of-breed BPaaS
-
End-to-end Best-of-breed BPaaS
-
Process-specific Best-of-breed BPaaS
-
-
-
Buyer Type Outlook (Revenue, USD Billion, 2018 - 2030)
-
Government Buyers
-
Medicare Advantage
-
Managed Medicaid
-
-
Commercial Buyers
-
Individual Health Plan
-
Employer-sponsored Health Plan
-
-
-
Value Chain Processes Outlook (Revenue, USD Billion, 2018 - 2030)
-
Claims Management
-
Member Engagement
-
Care Management
-
Others
-
-
Buyer Size Outlook (Revenue, USD Billion, 2018 - 2030)
-
Small Buyers
-
Midsized Buyers
-
Large Buyers
-
Frequently Asked Questions About This Report
b. The U.S. business process as a service in healthcare payers market size was estimated at USD 6.5 billion in 2023 and is expected to reach USD 6.9 billion in 2024.
b. The U.S. business process as a service in healthcare payers market is expected to grow at a compound annual growth rate of 5.62% from 2024 to 2030 to reach USD 9.6 billion by 2030.
b. The Traditional BPaaS solution dominated the U.S. business process as a service (BPaaS) in healthcare payers market with a share of 76.9% in 2023. This is largely due to the fact that a single provider offers an end-to-end one-stop traditional BPaaS solution, which acts as the most popular choice among payers and is catching up as a result of increased commercial SaaS use.
b. Some key players operating in the U.S. BPaaS in healthcare payers Market include Accenture; Cognizant; HCL; IBM; Infosys; NTT DATA; Optum; TCS; UST; Wipro; EXL; Softheon; Genpact; Change Healthcare; Firstsource; Celegence.
b. Key factors that are driving the market growth include the COVID-19 pandemic, expanding healthcare consumerism, changing regulations, and the shift to value-based healthcare.
Share this report with your colleague or friend.
![gvr icn]()
NEED A CUSTOM REPORT?
We can customize every report - free of charge - including purchasing stand-alone sections or country-level reports, as well as offer affordable discounts for start-ups & universities. Contact us now
![Certified Icon]()
We are GDPR and CCPA compliant! Your transaction & personal information is safe and secure. For more details, please read our privacy policy.
We are committed towards customer satisfaction, and quality service.
"The quality of research they have done for us has been excellent."