- Home
- »
- Healthcare IT
- »
-
U.S. Population Health Management Market Size Report 2033GVR Report cover
![U.S. Population Health Management Market Size, Share & Trends Report]()
U.S. Population Health Management Market (2025 - 2033) Size, Share & Trends Analysis Report By Product (Software, Services), By Delivery Mode (On-Premise, Cloud-based), By End Use (Providers, Payers, Employer Groups), By Region, And Segment Forecasts
- Report ID: GVR-2-68038-458-1
- Number of Report Pages: 100
- Format: PDF
- Historical Range: 2021 - 2023
- Forecast Period: 2025 - 2033
- Industry: Healthcare
- Report Summary
- Table of Contents
- Segmentation
- Methodology
- Download FREE Sample
-
Download Sample Report
U.S. Population Health Management Market Summary
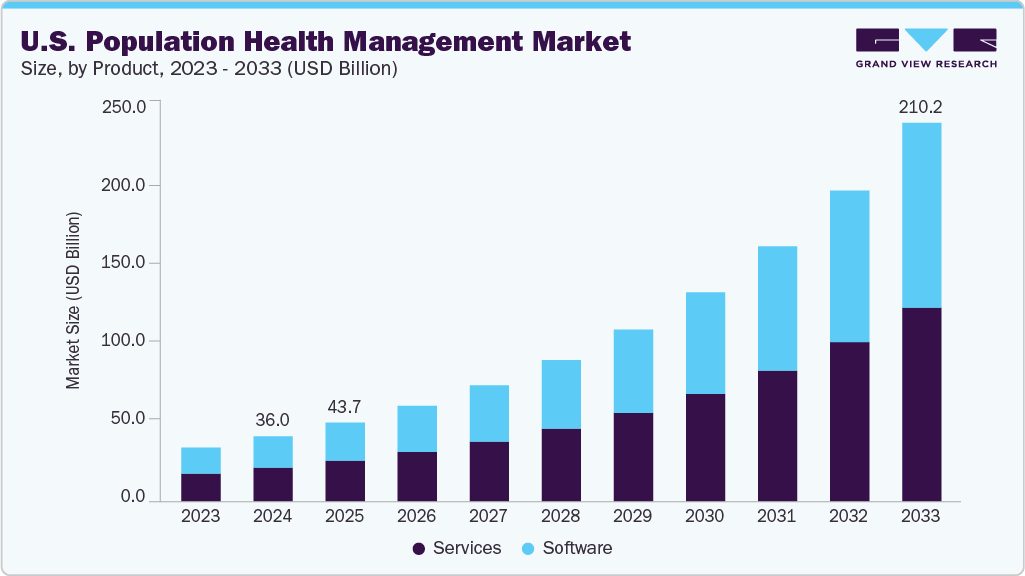
The U.S. population health management market size was estimated at USD 36.04 billion in 2024 and is projected to reach USD 210.18 billion by 2033, growing at a CAGR of 21.70% from 2025 to 2033. The market growth is majorly driven by the rising demand for healthcare IT services and solutions that support value-based healthcare delivery, resulting in a transition from Fee-For-Service (FFS) to a Value-Based Payment (VBP) model.
Key Market Trends & Insights
- Based on product, the services segment held the highest market share of 51.83% in 2024.
- Based on delivery mode, the cloud-based segment held the highest market share in 2024.
- By end use, the healthcare providers segment held the highest market share in 2024.
Market Size & Forecast
- 2024 Market Size: USD 36.04 Billion
- 2033 Projected Market Size: USD 210.18 Billion
- CAGR (2025-2033): 21.70%
Increasing healthcare expenditure, the rising need for value-based healthcare, and effective disease management across different care settings are expected to drive the growth of the U.S. population health management industry. More than 130 million people in the U.S. suffer from at least one chronic condition. For instance, according to the data published by the Centers for Disease Control and Prevention (CDC) in February 2024, an estimated 129 million people in the U.S. live with at least one major chronic disease.
Population health management solutions based on open Application Programming Interfaces (APIs) are helpful for the management of chronic conditions with high treatment costs, such as cardiac diseases, asthma, and diabetes. PHM solutions also help reduce the cost of care, improve patient outcomes. PHM software also enables better analysis of patient data to make informed decisions.
Moreover, the implementation of population health management (PHM) facilitates the identification of at-risk patients and enhances disease prevention and management, resulting in financial savings. The Centers for Medicare & Medicaid Services (CMS) has introduced the Value-Based Payment Modifier to promote the adoption of PHM systems. This modifier offers varying payment rates to physician groups based on the quality of care provided, rather than the cost of care incurred during their performance period.
In the U.S., providers, payers, and accountable care organizations promote PHM systems. Many providers and payers require upgrading and automating their healthcare management systems, which is anticipated to improve healthcare delivery and help departments collaborate. The providers mainly focus on chronic diseases, such as diabetes and cardiovascular disorders, which are generally responsible for significant healthcare costs. The rising prevalence of lifestyle disorders has increased the need for effective management of the disease burden on healthcare centers.
Furthermore, key players are engaged in strategic initiatives, such as the launch of new products, partnerships and collaborations, mergers and acquisition activities, etc., which contribute to market growth. For instance, in May 2025, Oracle, the Cleveland Clinic, and G42 announced a strategic partnership to develop an AI-based global healthcare platform. This platform will leverage AI, large-scale data analytics, and clinical expertise to deliver scalable, affordable care models, enhancing patient outcomes, precision medicine, and public health management across the U.S. and UAE.
“Aging populations, rising costs, and the complexity of care demand a complete reinvention of how healthcare is provided. Oracle’s AI Data Platform and suite of clinical applications can help us understand disease and population health in ways that fuel scientific breakthroughs, reduce the cost of care delivery, and improve patient care. Together with Cleveland Clinic and G42, we will deliver the modern tools providers need to help people live longer, healthier lives.”
-Oracle Executive Chairman and CTO Larry Ellison
Market Concentration & Characteristics
The chart below illustrates the relationship between industry concentration, industry characteristics, and industry participants. The x-axis represents the level of industry concentration, ranging from low to high. The y-axis represents various industry characteristics, including industry competition, level of partnerships & collaboration activities, degree of innovation, impact of regulations, and regional expansion. The U.S. population health management market is fragmented, with the presence of several emerging solution healthcare providers dominating the market. The degree of innovation and the level of merger & acquisition activities, and the impact of regulations on the industry are high. Moreover, the regional expansion of the market is moderate.
The U.S. population health management market experiences a high degree of innovation driven by technological advancements. The increasing adoption of artificial intelligence in PHM to enhance patient engagement, clinical documentation, and hospital administration supports innovations in the market. For instance, in October 2024, Microsoft leveraged its AI and analytical capabilities to harmonize information from CMS with clinical, SDOH, and imaging data for population health management.

The industry is experiencing a moderate level of partnerships & collaborations undertaken by several key players. This is due to the desire to gain a competitive advantage in the U.S. population health management industry, enhance technological capabilities, and consolidate in a rapidly growing market. For instance, in July 2025, MedeAnalytics and ZeOmega partnered to launch Population Health Navigator (PHN), a unified platform combining predictive analytics and care coordination.
Regulations, such as the HIPAA in the U.S. and the GDPR in Europe, establish standards for safeguarding patient data privacy and security. Compliance with these regulations is crucial for AI applications in healthcare to ensure the safe and secure handling of patient information, reducing the risk of data breaches and unauthorized access.
The U.S. population health management market is governed by federal healthcare reforms that promote value-based care and coordinated health delivery. Programs under the Affordable Care Act (ACA), including the Medicare Shared Savings Program (MSSP) and Accountable Care Organizations (ACOs), incentivize providers to adopt PHM solutions to improve outcomes while lowering costs. The Centers for Medicare & Medicaid Services (CMS) mandates quality reporting and risk adjustment models, making data-driven PHM tools essential for compliance. Moreover, the Health Insurance Portability and Accountability Act (HIPAA) protects patient data privacy and security, and the 21st Century Cures Act emphasizes interoperability and patient data access through standardized formats like FHIR.
Product Insights
The services segment held the largest market share of 51.83% in 2024. The PHM services help organizations design frameworks that align with value-based care models and regulatory requirements. Moreover, these services are essential for addressing interoperability challenges within population health initiatives. Service providers assist in integrating disparate electronic health record systems, claims databases, and health information exchanges. This ensures seamless data flow and enables comprehensive patient insights across care settings.
The software segment is expected to grow at the fastest CAGR during the forecast period due to the rising demand for advanced analytics and predictive modeling. Software platforms enable providers to aggregate and analyze data from electronic health records, claims systems, and patient monitoring tools. Predictive algorithms help identify at-risk populations and forecast disease progression, enabling timely interventions. These capabilities reduce hospital readmissions and improve long-term outcomes.
Delivery Mode Insights
The cloud-based segment led the U.S. population health management market with the largest revenue share of 72.03% in 2024 and is expected to grow at the fastest CAGR during the forecast period. The growth is attributed to its scalability and cost-effectiveness. Cloud-based platforms improve interoperability and data sharing across healthcare systems. They enable seamless integration of electronic health records, claims data, and remote monitoring inputs into unified dashboards. Real-time accessibility ensures care teams across multiple facilities collaborate effectively, improving coordination and outcomes. Compliance with federal interoperability mandates, including the 21st Century Cures Act, further supports the adoption of cloud-based systems. For instance, in July 2025, Johns Hopkins Health System launched Illustra Health, introducing a cloud-based population health analytics platform designed to enhance value-based care and support healthcare organizations in managing population health effectively.
Moreover, the web-based segment is expected to grow significantly over the forecast period. Web-based solutions require minimal infrastructure investment while offering broad accessibility through standard browsers. This makes them appealing for mid-sized hospitals, physician groups, and community health providers with budget constraints. Furthermore, the capacity to deliver centralized data access without complicated IT requirements facilitates adoption across various healthcare settings.
End Use Insights
The healthcare providers segment led the U.S. population health management industry with the largest revenue share of 47.81% in 2024. Healthcare providers need PHM systems that are compatible with electronic health record (EHR) systems to assist in delivering holistic, patient-centric care. Multiple functionalities and advantages offered by PHM solutions are responsible for their increased adoption. The Centers for Medicare & Medicaid Services has announced that the Alternative Payment Model and the Merit-Based Incentive Payment System will help these providers develop technical management capabilities.
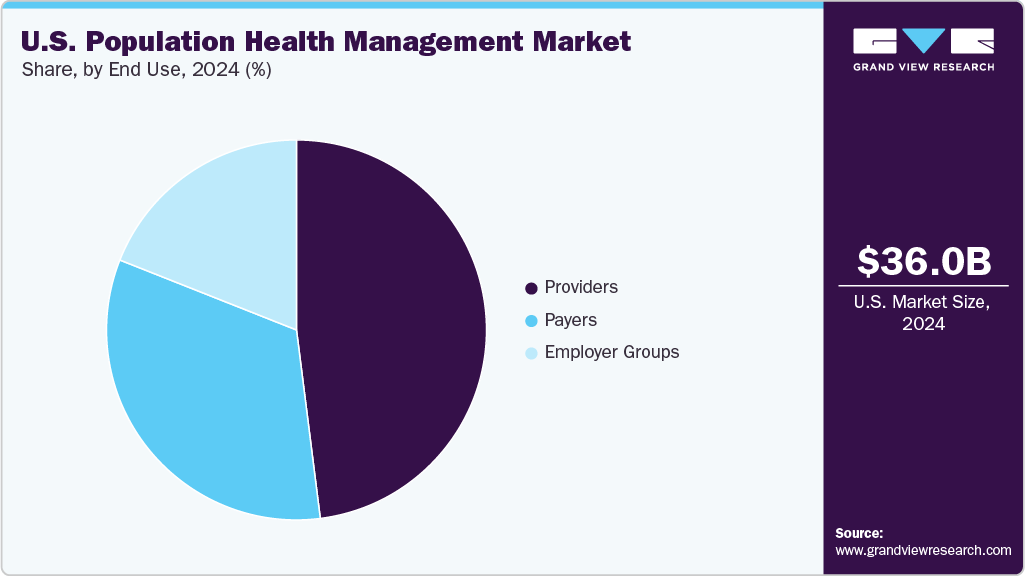
The employer groups segment is expected to witness the fastest CAGR over the forecast period due to the rising focus on employee wellness and healthcare cost containment. Employers are increasingly investing in PHM solutions to manage chronic conditions, reduce absenteeism, and improve workforce productivity. In addition, they are leveraging data-driven PHM tools to analyze claims, biometrics, and risk assessments, enabling proactive interventions.
Key U.S. Population Health Management Company Insights
Key players operating in the population health management market are undertaking various initiatives to strengthen their market presence and increase the reach of their products and services. Strategies such as new product launches and partnerships are playing a key role in propelling market growth.
Key U.S. Population Health Management Companies:
- Veradigm LLC.
- Oracle
- Conifer Health Solutions, LLC
- eClinicalWorks
- Enli Health Intelligence
- McKesson Corp.
- Medecision
- Optum, Inc.
- Advisory Board
- Koninklijke Philips N.V.
- athenahealth, Inc.
- RedBrick Health
- Welltok
Recent Developments
-
In January 2025, Percipio Health launched an AI-powered population health platform, securing USD 20 million in Series A funding led by UPMC Enterprises, WAVE Ventures, and Labcorp. The platform uses a smartphone app to collect vision-based and vocal AI biomarkers and other health signals, enabling real-time, device-free, holistic health monitoring and predictive insights for value-based care.
-
In November 2024, Emory Healthcare and Emory Healthcare Network launched a population health collaborative with GuideHealth, an AI-enabled value-based care services company. The collaboration is anticipated to focus on value-based care for over 350,000 individuals in Georgia.
-
In September 2024, AssureCare launched a real-time integration feature for its MedCompass platform, enabling seamless submission of prior authorization requests directly from EHRs. This advancement ensures compliance with CMS regulations, streamlining the prior authorization process and reducing administrative burdens for payors, ultimately enhancing efficiency in healthcare operations.
-
In September 2024, HealthEC and VirtualHealth partnered to integrate HealthEC’s advanced population health analytics with VirtualHealth’s HELIOS care management platform.
“We have an outstanding platform that we’ve developed into a single solution for end-to-end medical management. HELIOS is used by big players in both the payer and provider markets because it’s able to support coordinated care management, population health management, utilization management, FHIR interoperability, and more all in one place. By working with population health analytics leader HealthEC, HELIOS customers will be able to connect population health data on a deeper level and provide insights that lead to improved patient care and health outcomes.”
-Adam Sabloff, Founder and CEO of VirtualHealth
U.S. Population Health Management Market Report Scope
Report Attribute
Details
Market size value in 2025
USD 43.69 billion
Revenue forecast in 2033
USD 210.18 billion
Growth rate
CAGR of 21.70% from 2025 to 2033
Base year for estimation
2024
Historical data
2021 - 2023
Forecast period
2025 - 2033
Quantitative units
Revenue in USD million/billion and CAGR from 2025 to 2033
Report coverage
Revenue forecast, company ranking, competitive landscape, growth factors, and trends
Segments covered
Product, delivery mode, end use
Country scope
U.S.
Key companies profiled
Veradigm LLC; Oracle; Conifer Health Solutions, LLC; eClinicalWorks; Enli Health Intelligence; McKesson Corp.; Medecision; Optum, Inc.; Advisory Board; Koninklijke Philips N.V.; athenahealth, Inc.; RedBrick Health; Welltok
Customization scope
Free report customization (equivalent up to 8 analyst’s working days) with purchase. Addition or alteration to country, regional & segment scope.
U.S. Population Health Management Market Report Segmentation
This report forecasts revenue growth and provides an analysis of the latest trends in each of the sub-segments from 2021 to 2033. For this report, Grand View Research has segmented the U.S. population health management market report based on product, delivery mode, and end use:
-
Product Outlook (Revenue, USD Million, 2021 - 2033)
-
Software
-
Services
-
-
Delivery Mode Outlook (Revenue, USD Million, 2021 - 2033)
-
On-Premise
-
Cloud-based
-
-
End Use Outlook (Revenue, USD Million, 2021 - 2033)
-
Providers
-
Payers
-
Employer Groups
-
Frequently Asked Questions About This Report
b. The U.S. population health management market size was estimated at USD 36.04 billion in 2024 and is expected to reach USD 43.69 billion in 2025.
b. The U.S. population health management market is expected to grow at a compound annual growth rate of 21.70% from 2025 to 2033 to reach USD 210.18 billion by 2033.
b. The services segment dominated the U.S. population health management market with a share of 51.83% in 2024. This is attributable to the rising demand for post-purchase assistance for PHM solutions.
b. Some key players operating in the U.S. population health management market are Veradigm LLC. Oracle Conifer Health Solutions, LLC; eClinicalWorks; Enli Health Intelligence; McKesson Corp.; Medecision; Optum, Inc.; Advisory Board; Koninklijke Philips N.V.; athenahealth, Inc.; RedBrick Health; and Welltok.
b. Key factors that are driving the U.S. population health management market growth growing demand for healthcare IT services and solutions that support value-based healthcare delivery, resulting in a transition from Fee-For-Service (FFS) to a Value-Based Payment (VBP) model. In addition, increasing healthcare expenditure, the rising need for value-based healthcare, and effective disease management across different care settings are other factors driving market growth.
Share this report with your colleague or friend.
Need a Tailored Report?
Customize this report to your needs — add regions, segments, or data points, with 20% free customization.

ISO 9001:2015 & 27001:2022 Certified
We are GDPR and CCPA compliant! Your transaction & personal information is safe and secure. For more details, please read our privacy policy.
Trusted market insights - try a free sample
See how our reports are structured and why industry leaders rely on Grand View Research. Get a free sample or ask us to tailor this report to your needs.